
The practitioners at ACT Podiatry have the expertise to treat the whole spectrum of podiatric patients, including those with minor complaints to those with complex and difficult conditions. We recognise the importance of referral and will do so should a patient's condition fall outside of our expertise or should a multidisciplinary approach be required.
The Primary Foot Care Patient (skin and nail complaints)

Skin complaints (in the form of corns, callouses, dry, cracked or excessively moist skin and tinea pedis) are common to the foot. Nail conditions are also common including thickening, deformity and infection.
Even though there are a range of reasons for a person to undergo a primary foot care consultation, our objective remains the same, to provide comfort for our patients, improve the appearance of their feet and reduce their risk of a foot complication (ie - infection). Certain people (i.e. diabetics and rheumatoid arthritics) greatly benefit from regular treatment of this type.
Onychomycotic nails (fungal infected nails) are a common presentation to our practice. This condition is easy to contract but quite difficult to treat. In this picture note four infected nails and one healthy nail for comparison. Treatment options include primary foot care and oral/topical medications. Laser therapy is another option but this method of treatment is not provided by our practice.
The Sports Person (elite; recreational; beginner)

Sports people, particularly those participating in running or activities involving running, are subject to a whole variety of foot, ankle and lower limb complaints.
Our approach in managing the sports person is comprehensive.
A thorough medical history is critical, as is a thorough lower extremity musculoskeletal/biomechanical assessment. Treatment options may be varied depending upon the type of complaint and its severity.
Treatment options include:
- Prescription/custom made foot orthoses
- Prefabricated foot orthoses
- Paddings
- Strappings
- Footwear advice/alteration
- Oral anti-inflammatory/analgesic medications
- Injectable pain relief (local anaesthesia with or without corticosteroids)
- Walking boots
- Physical therapy (stretching exercises, strengthening exercises, proprioception exercises)
- Referral
- Medical Imaging (with or without corticosteroid injection)
- Other (ie: training modification including cross training)
- Surgery (reserved for patients who have failed to respond to other forms of care. Surgery may offer a definitive solution)
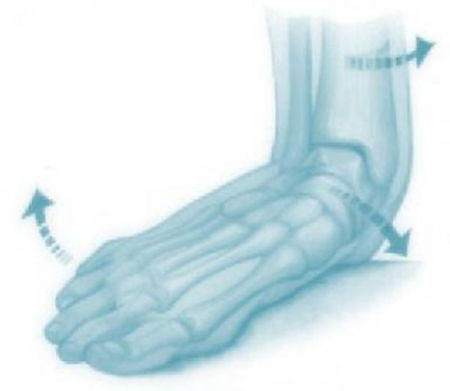
Over pronation or supination can adversely affect the sports person. Prescription made foot orthoses (custom made shoe inserts) are often highly effective at managing pain associated with abnormal foot motion.
Childrens (in-growing toe nails, plantar warts, flat feet, heel pain)
Common complaints for children include ingrowing toe nails, plantar warts, flat feet and heel pain. NB: All foot or leg pain in children should be appropriately investigated and will usually be treated.
Ingrowing Toe Nails: These can be managed through physical care whereby the ingrowing piece of nail is actually removed. Sometimes an antibiotic is necessary to address any persisting infection. This is not usually necessary because once the offending piece of nail is removed the inflammation and pain will settle. Persistent in-growing toe nails may be best addressed via surgery performed in the clinic. This is highly successful, relatively pain free and usually provides a permanent solution.
Plantar Warts: These are traditionally difficult to treat and a great deal of patience is required on behalf of the patient and parents. A definitive solution can be achieved via a curettage procedure but this is best done on isolated lesions. Mosaic warts (or multiple cluster warts) are more difficult to treat via curettage. They are best treated using cold or acid applications (i.e. salicylic acid) and through debridement (i.e. paring back) of the overlying skin followed by occlusive therapy (covering or smothering the warts with water tight/air-tight dressings). Our podiatrists can advise on the best method of treatment for your child.
Flat Feet (pes planus feet/abnormally pronated/excessively pronated/hyperpronated feet): This is a common condition presenting to our practice. There are two types physiologic (normal) and pathologic (abnormal). Flat feet associated with pain can be considered as pathologic. Pain free feet which are severely flat may also be considered as pathologic. Children often have physiologic flat feet where the arch is normal for their age and there is no associated pain. As such not all children with flat feet will require treatment. The various options of managing this complaint can be discussed with our practitioners following thorough medical and biomechanical/musculoskeletal assessments. Flexible flat feet usually exhibit a relatively normal arch during non-weight bearing but a low on weight bearing. The arch in a rigid flat foot (which is usually pathologic) is low on both weight and non weight bearing.
The flat foot condition usually responds very well to prescription made foot orthoses, deep and stable footwear and stretching of the calf muscles (triceps surae). In cases of a rigid flat foot the only effective treatment may be corrective surgery. Surgery may also be the best form of treatment in severe forms of flexible flexible flat feet.
Heel/Arch Pain: Paediatric patients are commonly afflicted with pain to the heel and arch. Children commonly present with flat feet, tight triceps surae (calf) muscles and are physically active. Boys present more frequently with these problems than girls. Heel and arch pain is common between the ages of 9-14 years of age but children of any age can be affected.
Knee/Patello-Femoral Pain: Sometimes children experience knee symptoms either in isolation or combination with other concerns (ie- flat feet, heel pain). Once more, prescription made foot orthoses, deep, stable footwear and strength/flexibility exercises are useful in reducing or eliminating these symptoms. Referral to a physiotherapist may be an important aspect of management addressing quadriceps (thigh) strength and core stability (abdominal strength).
Poor Posture: Children will often present to our practice because their parents are concerned about their body posture including their flat feet. Postural awareness should be developed as early as possible. Children with flat feet, inwardly turning knees, a sway back (lumbar lordosis) including a bottom which sticks out, round shoulders and a head which struts forward may benefit from a combination of podiatric and physiotherapy management.
Postural Fatigue: This refers to a generalised ache or pain affecting the feet, ankles and lower limb. This is very common in active children with flat feet. Some children avoid being active due to experiencing postural fatigue. The symptoms associated with this usually respond very well to prescription made foot orthoses, triceps surae stretching and deep and stable footwear. Sometimes children should consider non-weight bearing forms of physical activity (i.e. cycling or swimming) should they experience a severe form of this complaint.
Surgery for Children - Flat Foot Surgery:
Tarsal Coalition: A common cause of a rigid flat foot is a coalition (or bridge of fibrous tissue, bone or cartilage) between two bones in the hind foot. Removal of the bony bridge may be required to fully resolve the disorder. Sometimes a fusion of the affected bones is necessary but this is usually reserved for more chronic cases involving arthritic change.
Flexible Flat Foot Surgery: A large variety of techniques exist to address this type of flat foot. Almost all techniques will involve lengthening of the triceps surae (calf) muscles or Achilles tendon. Techniques which preserve joint surfaces are preferable to techniques involving joint fusion. Such surgery, if possible will need to be discussed in detail with our podiatric practitioners.
The Diabetic Patient
The diabetic person requires a very specific treatment approach due to their increased susceptibility to vascular disease, neuropathic changes (nerve changes, including sensory loss to the feet), foot deformity, ulceration and ultimately life threatening infection than other types of patients.
The diabetic should therefore manage their feet very carefully to prevent a foot complication such as ulceration, infection (to the soft tissues and or bone) and amputation of a toe, foot and even below the knee.
Management aims to reduce the risk of the patient developing a foot ulcer. This is done medically through good glycaemic control (achieved through medications including insulin, diet and exercise) and through appropriate podiatric screening and treatment as necessary.
Podiatric management involves:
Neurovascular Foot Assessment A neurovascular assessment is a powerful and accurate technique for determining the level of risk a patient has of developing a foot complication. The patient is profiled at low, moderate or high risk so that the potential need for introducing certain treatments options can be identified as soon as possible. The ACT Podiatry Annual Diabetic Assessment is an evidence based assessment tool, and Diabetes Australia recommends annual screening as a minimum to all our diabetic patients. Patients assessed to be at high risk from developing foot ulcers will be advised to consult with our podiatrists on a more regular basis so that their feet can be more closely monitored, and appropriate education can be provided to minimise this risk.
Primary foot care is the reduction of nails and hyperkeratotic skin (i.e. corns and callouses) improving comfort and reducing the risk of infection.
Nail surgery may be recommended to reduce ongoing infection risk associated with ingrowing toe nails
Orthomechanical treatments include footwear modifications or changes (shoes need to be comfortable, deep, wide and stable reducing pressure to the toes, plantar forefoot and bony prominences). Prescription made foot orthoses may also be recommended to reduce pressure points on the plantar (sole) of the foot, improve balance and reduce abnormal motion or position of the feet.
Foot surgery can be used to directly treat abscess formation and bone infection or to treat deformities which can increase the likelihood of these infections. This is termed reconstructive foot surgery which is commonly performed on the diabetic patient to reduce their risk profile.
We provide health education and advice We provide health education and advice
Diabetes Australia provides valuable resources for people with diabetes.
The Arthritic Patient (inflammatory arthritis/osteoarthritis)
Osteoarthritis is the most common arthritic complaint in the community and can affect all the joints of the feet. Inflammatory arthritis, such as rheumatoid arthritis is less common but can lead to progressive cartilage loss and joint damage similar to osteoarthritis. Patients with inflammatory arthritis can be immunosuppressed increasing the risk of infection and decreasing their capacity for wound healing.
All our treatment options can be used to manage patients with foot and ankle arthritis. Treatment options depend upon the degree of pain associated with the disease, the extent of cartilage loss and joint damage, and the impact the arthritic joint/s has on mobility and quality of life. Non-surgical forms of treatment can work very well for most people with arthritic feet. Some people require surgery to eliminate or reduce pain, restore alignment and improve mobility/quality of life.
It is common for people with arthritis to have hallux rigidus (big toe joint arthritis), hammer/claw toes, and bony lumps/bumps on their feet. People with arthritis often experience pain to the ball of the foot.
Arthritis Australia provides useful information for people with arthritis.
foot and ankle conditions
- Hallux Valgus (Bunions – progressive dislocation of the big toe joint)
- Hallux Rigidus (Osteoarthritis of the big toe joint)
- Hammer/Claw Toes
- Plantar Forefoot Pain
- Heel Pain (including plantar fasciitis/plantar fasciopathy)
- Bumps and Lumps (bony and soft tissue)
- Arthritis (forefoot, midfoot, rearfoot and ankle)
- Complex foot and ankle complaints (patients with multiple concerns)
- Ingrown Toenail Surgery
- Something Unusual
faq
- What are Podiatrists & Podiatric Surgeons?
- What is the point of difference between
ACT Podiatry and other practices? - What are common forefoot conditions
treated at ACT Podiatry? - What are common mid-foot and rear foot
conditions seen at ACT Podiatry? - What predisposes a person
to lower limb pain - What are foot orthoses?
- Can a spinal condition cause foot pain?
- Is arterial disease a cause of foot pain?
- I am diabetic and my feet burn
– what is this? - Can in-growing toe nails and plantar warts be cured?
Suite 8 (Ground Floor), 146 Scollay St, Greenway ACT 2900
6287 4889
6293 2325
[email protected]
ACT Podiatry : Advanced Foot & Ankle Centre
Canberra Podiatric Surgeon
Suites 16-17 (First floor) 14-16 Brierly St, Weston ACT 2611
6287 2818
6293 2325
[email protected]
ACT Podiatry : Advanced Foot & Ankle Centre
Canberra Podiatric Surgeon
Copyright © 2018, ACT PODIATRY | SEO by High Jump Digital


