
There are many disorders which affect the feet, ankles and legs. Some of these we are born with, some are associated with hereditary, many develop as we age, some are associated with specific medical conditions and some are caused by trauma or infection. ACT Podiatry is dedicated to recognise these conditions and their causes so we may improve the health of your feet and in turn, your mobility and quality of life. We use proven techniques and treatment modalities to ensure you receive the best possible care.
Hallux Valgus (Bunions - progressive dislocation of the big toe joint)
This disorder is a progressive dislocation of the 1st metatarsophalangeal joint (big toe joint) and is primarily inherited. It is commonly associated with pain and osteoarthritis of this particular joint as well as progressive subluxation of the lesser metatarsophalangeal joints (small toe joints) leading to progressive hammer/claw toes and associated plantar (bottom of the forefoot) pain. Corn and callouses are common consequences of a foot afflicted with hallux valgus. Nerve entrapments (ie-neuromas) exhibit a high incidence in patients exhibited a hallux valgus deformity. Patients with hallux valgus often experience a reduction in quality of life, mobility and experience foot wear fitting difficulties.
Hallux valgus and its associated complaints can be treated in many cases without surgery depending upon the severity of the disorder. Primary foot care can be used to address corns and callouses and thickened/ingrowing toe nails associated with it. Foot orthoses can be used to reduce pressure to the foot and control foot pronation commonly associated with its development or progression. Shoes can be used to accommodate ‘bunions’ and reduce pressure from the top of the lesser toes. Medications can be a useful compliment to these measures.
Hallux valgus surgery is reported in the literature as highly reliable at treating this condition when other forms of treatment have proven ineffective or in more advanced cases where conservative care (ie – non-operative management) is not indicated. There are many types of potential procedures which can be performed and these options can be discussed with our practitioners.

Hallux valgus (bunions) usually worsen over time.
To see a graphic of hallux valgus surgery (video one) please click below.
Hallux Rigidus (Osteoarthritis of the big toe joint)
This disorder is a progressive osteoarthritic change, taking place at the 1st metatarsophalangeal joint. It has been associated with many possible causes. It can be post-traumatic (ie-secondary to injury) but it often isn’t. The rheumatoid arthritic and diabetic patient are more prone to developing this condition but it has a broad based prevalence. As with hallux valgus patients with hallux rigidus often experience a reduction in quality of life, mobility and experience foot wear fitting difficulties.
Hallux rigidus can be managed quite well in the early stages with foot orthoses and appropriate footwear. However, once the range of motion reduces significantly then conservative management (ie-non-surgical) proves far less effective. The extent of damage can be assessed by plain film radiograph evaluation (x-rays), range of motion studies and the use of quality of life measurement tools such as the Foot Health Status Questionnaire. As with hallux valgus surgery a large variety of techniques exist to address the pain and disability associated with this complaint. Such technique may preserve the joint, reconstruct the joint or be joint destructive. Each of these options can be discussed with the appropriate procedure selected based on the extent of the joint disease process and preference of the patient.
A technique called a capsular interpositional arthroplasty procedure is commonly used by podiatric surgeons preserving as much range of motion as possible whilst eliminating pain. An arthrodesis procedure (ie- joint fusion with or without a graft - video three) is reported by the literature as achieving excellent reduction in pain but it completely eliminated range of motion of the joint. This may not be a preference for some patients and should be discussed with our practitioners.
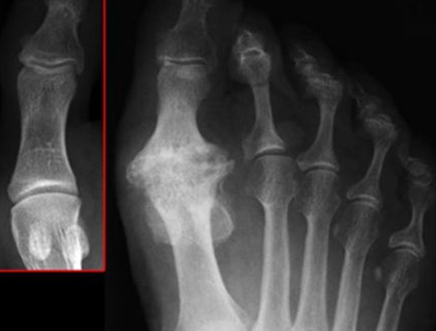
This plain film radiograph (x-ray) demonstrates a normal joint in comparison with a severe case of hallux rigidus.
An arthrodesis procedure with/without a bone graft can be an effective means of treating hallux rigidis. Please click below (video two) to see a simple example of this procedure.
Hammer/Claw Toes
These may occur in isolation or may affected multiple toes involving both feet (see below picture). People afflicted with claw toes commonly experience corns and callouses to the tips and dorsum (top) of the toes and to the plantar (bottom) of the forefoot. In severe cases the fat pad which protects the joints of the plantar forefoot (lesser metatarsophalangeal joints) is displaced distally (ie- shift towards to toes and off the joints) leaving them exposed and painful. Patient with rheumatoid arthritis and diabetes have a higher incidence of claw/hammer toes.
Hammer toes can be treated in many cases without surgery depending upon the severity of the complaint. Primary foot care can be used to address corns and callouses and thickened/ingrowing toe nails associated with hammer/claw toes. Foot orthoses can be used to reduce pressure to the plantar forefoot (ball of the foot). This pressure is commonly associated with hammer/claw toe formation often caused by an acute or progressive tear of the plantar plate. Shoes can be used to accommodate hammer/claw toes and reduce pressure from the top of the lesser toes. Medications can be a useful compliment to these measures.
Surgery can be used to straighten toes, eliminate corns and callous associated with them and reduce pain. The straightening of toes is important in the diabetic and rheumatoid patient as they will be more susceptible to infection because of localised tissue trauma and potential ulceration. Once the protective layer of skin is breached a portal of entry is provided to bacteria leading cellulitis (soft tissue infection) and/or osteomyelitis (bone infection).
Digital surgery (corrective toe surgery) is complex and many techniques exist to straighten toes. Such techniques can be discussed with our practitioners.

Hammer toes are commonly caused by progressive or acute rupture of the plantar plate (video three). There are a number of surgical methods used to correct claw/hammer toe deformities (video four). Please click below to see an explanation of the plantar plate rupture and to see a simple example of a hammer toe corrective procedure.
Plantar Forefoot Pain
This is commonly associated with hallux valgus (bunions), claw/hammer toes and localised nerve entrapment conditions called Morton’s or intermetatarsal neuromas.
Each of these conditions can be addressed surgically should conservative methods of treatment prove ineffective.
Neuromas (forefoot nerve entrapment)
These are very common to the forefoot (front part of the foot) but can be difficult to diagnose and are often misdiagnosed. Neuromas present clinically, with a wide range of signs and symptoms. They may be first noticed as a very intermittent sharp shooting pain in the forefoot and at times into the lesser digits (small toes of the foot). As the condition progresses this pain becomes more intense and more frequent. Patients often experience their symptoms more often or to a greater extend in tighter fitting footwear so women will often present to our clinic. As the condition becomes more severe burning is experienced to the plantar forefoot (ball of the foot) with sharp shooting pains into the lesser toes (usually the 3rd and 4th toes and less of the 2nd and 3rd toes) with a description of nerve type pain (ie-paraesthesia) including numbness. In the early stages neuromas can be managed very well non-surgically. Effective forms of treatment included wider more stable shoes, prescription made foot orthoses (with or without metatarsal padding) and injection therapy (local anaesthesia with/without corticosteroid). Topical and or oral anti-inflammatories or analgesics (pain killers) can be useful temporarily but are rarely useful in the long term. Larger and more severe neuromas may often only be resolved definitively with surgery known as a neurectomy procedure.
In this technique the disease portion of nerve is resected. This leaves an area of permanent numbness, which gradually reduces in size over time so it becomes barely noticeable. Usually patient have numbness affected the relevant toes by the time they require this form of treatment. Numbness between the affected toes is an effective diagnostic technique to assess for the presence or otherwise of a neuroma.
Please click below (video five) for a brief explanation about neuromas and to see a simple example of how surgery can be used to treat this condition.
Heel Pain (including plantar fasciitis/plantar fasciopathy)
This is likely the most common affliction of the human hind or rear foot. The vast majority of cases respond to non-surgical intervention. Prefabricated and custom-made foot orthoses resolve the majority of cases and can be used to prevent a recurrence of the complaint. Oral or topical anti-inflammatory in conjunction with stretching and RICE (rest-ice, compression and elevation) are useful adjunctive forms of treatment. Strappings can be used for heel pain both diagnostically and therapeutically. That is a patient responding well to a strapping through a reduction in pain and an increase in support will usually respond well to orthotic therapy.
More severe cases of plantar fasciitis may require more intensive care involving the temporary use of walking boots and injection therapy (see information section). This is usually reserved for patients who have considerable pain and have great difficulty placing weight through their heel. Surgery is used for patients who do not respond to non-surgical management. Remember the vast majority of people with plantar fasciitis/plantar fasciopathy or or heel pain affecting the inside of the heel and arch will respond to non-surgical management.
Surgery commonly consists of two techniques – the plantar fasciotomy and the plantar fasciectomy (with or without heel spur resection). Sometimes heel pain has a ‘nerve component’ and surgery of this type is combined with posterior tibial nerve decompression but this is not commonly performed.
Our practitioners can discuss each of these treatment options with you. Prescription medication can be prescribed as required.
For a brief overview of plantar fasciitis (plantar fasciopathy) including treatment options, please click below (video six).
Bumps and Lumps (bony and soft tissue)
Bony protubences and bumps commonly affect the feet. In most cases bumps are caused by arthritic changes and are reflective of peri-articular spurring or spurring around a joint. Sometimes a bump may be associated with a soft tissue lesion such as a ganglionic cyst, plantar wart and in more serious cases an abscess which is most likely to be seen in the diabetic foot.
Bumps and protrubences may or may not cause a problem in which case most can be left alone. However commonly they need to be addressed. They may be accommodated by wearing deeper and wider footwear or padded to prevent the overlying skin and actual lesion from being irritated. In many cases soft tissue lesions such as ganglions need to be excised. Spurring around joints can also be removed surgically. Surgery can provide great relief from irritation and pain.
Arthritis (forefoot, midfoot, rearfoot and ankle)
Arthritis can affect any joint in the human body and all the joints of the foot can be affected in addition to the ankle. The extent and location of arthritis will determine which treatment options are to be used. Orthotic therapy, physical therapy, pharmacology (medications) and sometimes injection therapy are important non-surgical methods of treatment.
Surgery is reserved for patients who do not respond well to conservative (non-surgical) methods of treatment. A pan metatarsal head resection procedure (or removal of all of the lesser metatarsal heads) is commonly preformed in rheumatoid arthritic patients with lesser metatarsophalangal joint pain, deformity and arthritis. In general the type of surgery will depend upon the level of pain the patient’s experiences and the extent of articular (ie-joint) damage. Joint preservation, joint reconstructive and joint destructive procedures all have a place in the treatment of arthritis.
Complex foot and ankle complaints (patients with multiple concerns)
The foot, ankle and lower limb are complex anatomical structures. A review of the bones of the foot alone (excluding all other structures such as blood vessels, nerves, tendons, ligaments etc) and how they function in movement (ie-pronation and supination) clearly demonstrates the level of complexity (videos eight and nine).
As such it is not uncommon for patient to present with multiple sites of pain or concern. This can be associated with patients with systemic disease such as diabetes and inflammatory arthritis (ie - rheumatoid arthritis) where their condition can affect multiple joints. Patients who have suffered a previous trauma (ie- motor vehicle accident or large fracture) may be placed in this category. Such people can benefit greatly from a detailed assessment and management. Often multiple practitioners are required to achieve the best outcomes. In terms of treatment is often best to differentiate the most painful site from the least and to treat accordingly.
Something Unusual
Many other complaints and therefore non-surgical/surgical techniques exist to address the full range of foot and ankle complaints.
foot and ankle conditions
- Hallux Valgus (Bunions – progressive dislocation of the big toe joint)
- Hallux Rigidus (Osteoarthritis of the big toe joint)
- Hammer/Claw Toes
- Plantar Forefoot Pain
- Heel Pain (including plantar fasciitis/plantar fasciopathy)
- Bumps and Lumps (bony and soft tissue)
- Arthritis (forefoot, midfoot, rearfoot and ankle)
- Complex foot and ankle complaints (patients with multiple concerns)
- Ingrown Toenail Surgery
- Something Unusual
faq
- What are Podiatrists & Podiatric Surgeons?
- What is the point of difference between
ACT Podiatry and other practices? - What are common forefoot conditions
treated at ACT Podiatry? - What are common mid-foot and rear foot
conditions seen at ACT Podiatry? - What predisposes a person
to lower limb pain - What are foot orthoses?
- Can a spinal condition cause foot pain?
- Is arterial disease a cause of foot pain?
- I am diabetic and my feet burn
– what is this? - Can in-growing toe nails and plantar warts be cured?
Suite 8 (Ground Floor), 146 Scollay St, Greenway ACT 2900
6287 4889
6293 2325
[email protected]
ACT Podiatry : Advanced Foot & Ankle Centre
Canberra Podiatric Surgeon
Suites 16-17 (First floor) 14-16 Brierly St, Weston ACT 2611
6287 2818
6293 2325
[email protected]
ACT Podiatry : Advanced Foot & Ankle Centre
Canberra Podiatric Surgeon
Copyright © 2018, ACT PODIATRY | SEO by High Jump Digital

